Statement – Cancer services disrupted by up to 50% in all countries reporting: a deadly impact of COVID-19
The European Region has recorded 12 million new [COVID-19] cases in the past week. This is the highest weekly case incidence since the start of the pandemic and is largely being driven by the highly transmissible Omicron variant, as it sweeps from west to east.
30% of all COVID-19 cases since the pandemic began have been reported this year alone. We now have nearly 150 million reported cases of COVID-19 in Europe and central Asia to date. 22% of all tests recorded are positive.
Hospitalizations continue to rise, mainly in countries with lower vaccination uptake in vulnerable populations. This rise, however, is not as rapid as the case incidence rate – and overall, admissions to intensive care have not increased significantly. For now, the number of deaths across the Region is starting to plateau.
I wish to reiterate the firm call I made last week, which is indeed referring to a plausible endgame for the pandemic – not to say that it is now all over – but to highlight that in the European Region, there is a singular opportunity to take control of the transmission because of the congruence of three elements:
- a large capital of vaccine derived and natural immunity to Omicron;
- a favourable seasonality pause as we move out of the winter; and
- the lower severity of the Omicron variant, now well established.
This context, that we have not experienced so far in this pandemic, leaves us with the possibility for a long period of tranquillity and a much higher level of population defence against any resurgence in transmission, even with a more virulent variant. This period of higher protection should be seen as a “ceasefire” that could bring us enduring peace, on the condition that we:
- consolidate and preserve immunity by keeping on vaccinating and boosting;
- focus on the 5 stabilizers for the most vulnerable, with strong governmental oversight and commitment;
- promote self-protecting behaviour and individual responsibility – here with lower governmental oversight to limit unnecessary socioeconomic impacts;
- intensify surveillance to detect new variants.
I believe that it is possible to respond to new variants that will inevitably emerge without re-installing the kind of disruptive measures we needed before.
And it is because we see that opportunity, that the top priority is to bring all countries to a level of protection which allows them to grasp this opportunity too, and look ahead towards more stable days. But this demands a drastic and uncompromising increase in vaccine-sharing across borders. We cannot accept vaccine inequity for one more day – vaccines must be for everyone, in the remotest corner of our vast Region and beyond.
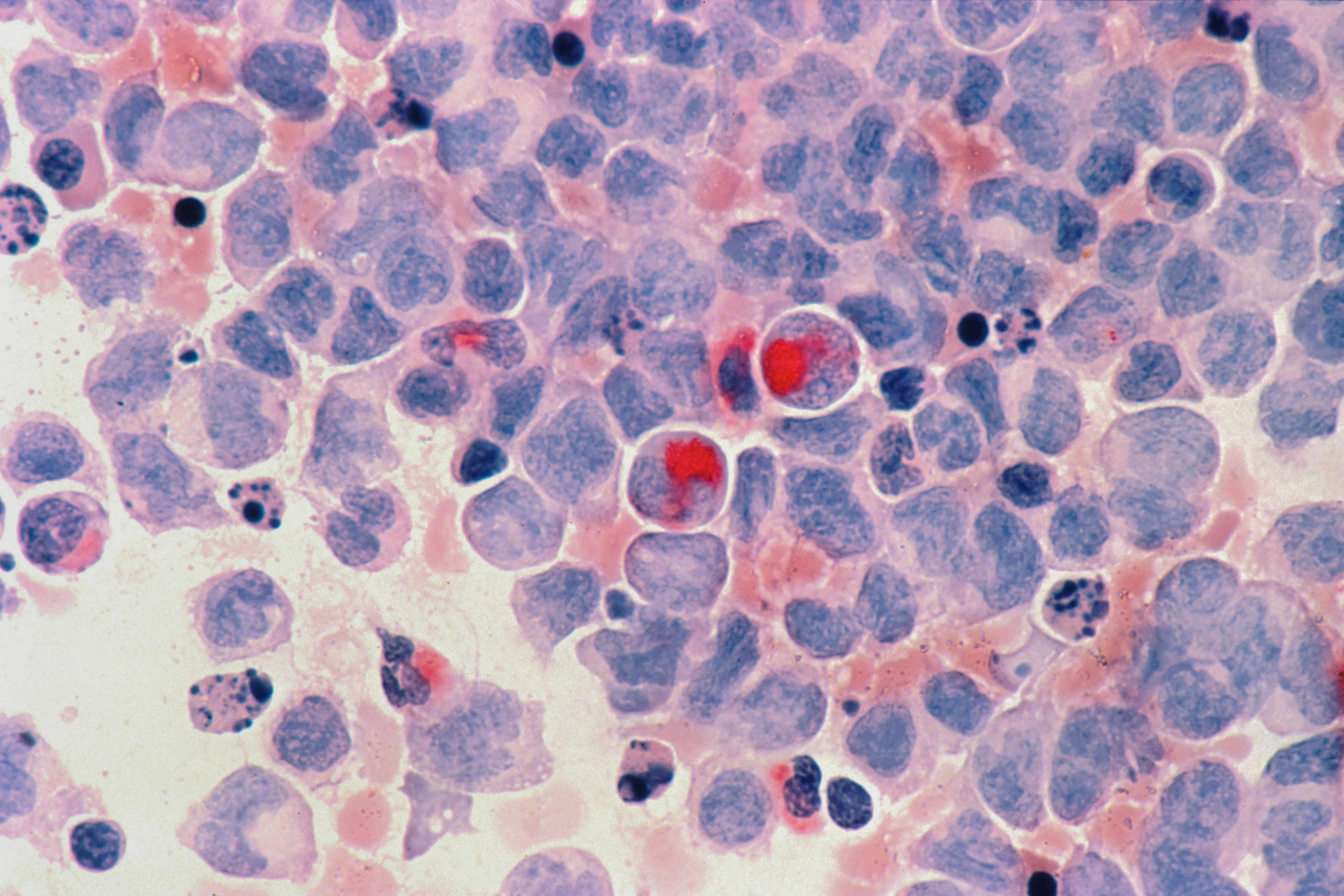
Tomorrow is World Cancer Day, and I want to take the opportunity to underscore the catastrophic impact the pandemic has had over the past 2 years on people with cancer. The impact of COVID-19 indeed goes far beyond the disease itself. Cancer touches all our lives, either directly or through its effect on family and loved ones. 1 in 4 people in Europe and central Asia will receive a cancer diagnosis in their lifetime. It is one of the leading causes of mortality and morbidity in the WHO European Region, accounting for more than 20% of all deaths.
Looking back over these past 2 years, cancer screening, diagnosis and treatment have suffered in an unprecedented way as health services have struggled to respond to COVID-19.
Consider this:
- during the early stages of the pandemic, the diagnosis of invasive tumours fell by 44% in Belgium*;
- in Italy, colorectal screenings decreased by 46% between 2019 and 2020**;
- in Spain, the number of cancers diagnosed in 2020 was 34% lower than expected***.
The latest Global Pulse Survey – conducted by WHO on the continuity of essential health services during the COVID-19 pandemic – indicates that in the last quarter of 2021 there was a disruption in cancer care – screening and treatment – of between 5 to 50% in all countries reporting. The situation has improved since the first quarter of last year, where services were disrupted by more than 50% in 44% of countries, and by between 5 to 50% in the rest, but the knock-on effect of this disruption will be felt for years.
44% of countries around the world reported an increase in service backlogs for cancer screening in the second half of 2021.
The way in which the pandemic delays cancer care and creates service backlogs is a deadly interplay.
At this point in time, 24 months since COVID-19’s arrival, the health workforce is overstretched and exhausted – repurposed to address the direct impact of the virus. But any respite that widespread immunity provides thanks to vaccination and in the wake of the less severe Omicron [variant], together with the coming spring and summer seasons, must be used immediately to enable health workers to return to other important health care functions in order to bring backlogs for chronic care services down. As we go forward, maintenance of essential health services, including services along the continuum of cancer care – from prevention to early detection, diagnosis, treatment and palliative care – must be a component of emergency planning and response.
World Cancer Day tomorrow, is a timely reminder that 30–40% of cancers in Europe and central Asia are preventable. To mark the day, we are publishing a new guide on cancer screening, summarizing evidence and ethics, and addressing misconceptions. This is part of an initiative we introduced a year ago – United Action Against Cancer – a commitment by WHO to fast track the elimination of cancer as a life-threatening disease in Europe and Central Asia – through cost-effective, evidence-based policies at every point of cancer care.
From where we stand now, as we see cases surge across Europe and central Asia, we remain at a critical juncture. But I remain optimistic that if we use the circumstances before us, we have the opportunity to experience more stable days ahead – a time when we will be able to not only manage COVID-19, but also have the capacity to address other urgent health priorities.
I am very happy to now introduce Aron Anderson, who is WHO/Europe’s Cancer Ambassador – a driving force in our initiative, United Action Against Cancer.